Go offline with the Player FM app!
Episode 019 — Shapeshifters and suspension
Archived series ("Inactive feed" status)
When?
This feed was archived on November 22, 2020 08:09 (
Why? Inactive feed status. Our servers were unable to retrieve a valid podcast feed for a sustained period.
What now? You might be able to find a more up-to-date version using the search function. This series will no longer be checked for updates. If you believe this to be in error, please check if the publisher's feed link below is valid and contact support to request the feed be restored or if you have any other concerns about this.
Manage episode 261970428 series 2505075
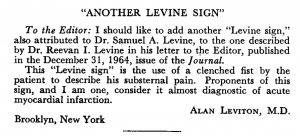
Levine sign
Oldest reference I can find is NEJM 1965:
NEJM, 1965 ( https://www.nejm.org/doi/full/10.1056/NEJM196502042720521 )
Preload, Afterload, & Inotropy → Nitroglycerin Clinical Pearl
Nitroglycerin
- “At modest doses, this effect occurs predominantly in the venous circulation, resulting in increased capacitance and a marked reduction in preload. This contributes to a partial off-loading of the ventricle with a reduction in end-diastolic volume and a decrease in pulmonary capillary wedge pressure (PCWP). At higher doses (i.e, ≥ 150–250 mcg/min) arteriolar dilatation occurs which helps to improve cardiac output through a reduction in afterload and diminished impedance to forward flow.” → https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821770/
Suspension Syndrome
A summary by Alex:
Essentially people get suspended in either mountaineering or industrial accidents and they end up dangling from a harness. When they are rescued they are fine, and then suddenly, usually minutes to days later, they die suddenly. It seems as though people have to be suspended for a few hours for this phenomena to occur.
Here’s the thing, you can read a bunch of papers that confidently assert why this occurs, but no one really knows for sure.
Theories as to why this happens:
1. Volume overload/myocardial rupture- the idea being that you lie them down, and then the blood rushes to the heart and overloads it as there is evidence that mechanical stretch + regional ischemia can cause arrhythmia. BS, these people are hypo or euvolemic, and they really don’t end up with overload, also since these people are more likely to have global hypoxia than local ischemia Pressure needed to actually rupture a healthy (lamb) heart is 526 mmHg. Assuming the person has a healthy heart (no recent MI), than it is very unlikely that one could actually cause this level of pressure to be reached. Hypovolemia requires loss of pretty significant amounts of blood, even at 15% the average healthy person will be pretty much normal. By 30-40% you see serious changes. I guess we can assume that hypervolemia requires similar levels of fluid changes to cause issues on a similar scale.
2. a) Bad blood coming back- immobile legs get hypoxic due to decreased venous return (you need to twitch the small muscles in your legs to avoid this). One theory is that this causes acidosis (which does happen 2 hrs s/p tourniquet a legs venous pH will be 6.9). That said, acidosis transiently decreases cardiac contractility, and really doesn’t cause arrhythmia. It could theoretically cause cariogenic shock, but this seems unlikely as this doesn’t match well with the clinical presentation of suspension syndrome patients.
b) The other side of the “bad blood” argument is potassium leak. This makes more sense and has been seen in crush cases (and the thought is that the physiology is overall pretty similar). That guy had his legs crushed for 8 hours, then had a pH of 7.15 (bad but not awful), and a K of 8 (BAD). He arrested, but they got him back (with what?! bicarb, insulin and glucose which we will discuss later).
So what do you do to treat these people?
In the field: Get access to them, then position them in Fowlers at 30-40 degrees, then slowly lower them to supine. Get ready to treat for complications (EKG, electrolytes, etc). If they have 10+ min of suspension they need to go to an ED. If they have even the most minor signs or symptoms, such as numb legs or transitory respiratory or circulatory problems they need to be admitted on telemetry.
Sources:
- Parker KK, Lavelle JA, Taylor LK, Wang Z, Hansen DE. Stretch-induced ventricular arrhythmias during acute ischemia and reperfusion. J Appl Physiol. 2004; 97:377–383.
- Lyon, Ross T., et al. “Myocardial Rupture: III. Chamber Pressure, Rate of Distention, and Ventricular Disruption in Isolated Hearts.” The Annals of Thoracic Surgery. 1979. doi:10.1016/s0003-4975(10)63369-3.
- Raynovich, Bill. “Dangerous Suspension: Understanding Suspension Syndrome & Prehospital Treatment for Those at Risk.” Journal of Emergency Medical Services. 2009.
- Bishop PA , JB Church: “An alternative mechanism for death by crucifixion.” Linacre Quarterly (J Catholic Medical Assn). 73(3):282Ï289, 2006.
Vocab
Protean (as in “tending or able to change frequently”)
- Schwartz’s Principles of Surgery: “Virtually any organ can become infected, giving rise to the protean manifestations of tuberculosis.”
- Cope’s Early Diagnosis of the Acute Abdomen: “The physician who wishes to be prepared thoroughly to examine and correctly diagnose patients with acute abdominal pain must be fully conversant with these diseases and their protean manifestations.
- Emergency Medicine, Avoiding the Pitfalls and Improving the Outcomes: “Clinical manifestations of SVC syndrome are protean and depend on the degree of vena cava obstruction.”
Step1 Q
A 30 y.o. M is brought to the ED after being the restrained driver in a motor vehicle accident. On physical examination, there is extensive bruising on his chest and abdomen, but no lacerations or open wounds. Blood pressure is 90/55 with a pulse of 122 bpm. On inspiration, his blood pressure is 70/50. On cardiovascular exam, his heart sounds are muffled and he has distended neck veins. What will be a pertinent finding on EKG to support this patient’s diagnosis?
(A) ST elevations in leads II, III, and aVF
(B) Irregularly irregular rhythm without discernible p-waves
(C) QRS complexes that alternate in height
(D) Diffuse ST elevation with PR depression
(E) S wave depth V1 + tallest R wave in V5-V6 > 35 mm
*Pulsus paradoxus
*Beck’s Triad
*Electrical alternans
*Equalization of all chamber pressures –> bad news!
EBM
“BiDil”
- Combo pill for heart failure → isosorbide dinitrate (20mg) and hydralazine (37.5mg)
- First drug approved to treat a general condition in patients of a specific race (and has been criticized as lending credence to the misperception of race as a biological category than social one)
- Approved after 3 trials:
- V-HeFT I → n=459 → no significant difference in all-cause mortality between the treatment group and placebo → post-hoc analysis showed benefit for self-identified African American patients
- V-HeFT II → n=804 → compared BiDil to enalapril → BiDil was found inferior to enalapril → post-hoc analysis showed self-identified racial subgroup (n=215) to have no significant difference (vs inferior for others)
- A-HeFT → n=1050 self-identified black men and women (across 169 US sites) → randomized to receive either BiDil (n=518) or placebo (n=532) for up to 18 months (+ background therapy) → Result was significant efficacy in a composite score of all-cause mortality, first hospitalization for HF, and the Minnesota Living with Heart Failure (MLHF) questionnaire. The drug was associated with a 43% relative reduction in all cause mortality and 8% absolute reduction in first-hospitalizations (16.4% vs. 24.4%).
- NYTimes 2005, Maker of Heart Drug Intended for Blacks Bases Price on Patients’ Wealth → “…set the price of its heart-failure drug BiDil at $1.80 a pill, significantly higher than what analysts had expected and nearly twice as much as some other heart-failure treatments. Depending on the dosage, that would make the cost of taking BiDil at least $5.40 and maybe as much as $10.80 a day.”
One other race based thing to note: even though BiDil was a commercial flop, there are other ways that race is employed in guidelines and modern practice, often perhaps without any better “scientific” backing — that is, maybe it’s just a proxy for something. I would encourage you to always at least question what the role of race is (when you encounter it in guidelines), and look for the science that supports its use. Race is used nowadays in the JNC 8 (2014) and 2017 AHA guidelines, which advise starting hypertensive African American patients on a CCB/thiazide rather than ACEI. We don’t have the space to open that entire can of worms here, but it’s worth noting that all of this relies on the 2002 ALLHAT study. The discussion section of the 2015 study linked below [which is a chart review with “okay” methodology] summarizes the evidence reasonably well.
“Although diuretics or CCBs are recommended as first-line agents in African-American patients, we found no significant difference in the optimal control of blood pressure and frequency of end-organ damage compared to management with other agents.” https://www.ncbi.nlm.nih.gov/pubmed/26713289
— Episode credits —
Hosted by Addie, Kim, and Alex. Audio production and editing by Addie. Show notes written by Addie and Alex.
21 episodes
Archived series ("Inactive feed" status)
When?
This feed was archived on November 22, 2020 08:09 (
Why? Inactive feed status. Our servers were unable to retrieve a valid podcast feed for a sustained period.
What now? You might be able to find a more up-to-date version using the search function. This series will no longer be checked for updates. If you believe this to be in error, please check if the publisher's feed link below is valid and contact support to request the feed be restored or if you have any other concerns about this.
Manage episode 261970428 series 2505075
Levine sign
Oldest reference I can find is NEJM 1965:
NEJM, 1965 ( https://www.nejm.org/doi/full/10.1056/NEJM196502042720521 )
Preload, Afterload, & Inotropy → Nitroglycerin Clinical Pearl
Nitroglycerin
- “At modest doses, this effect occurs predominantly in the venous circulation, resulting in increased capacitance and a marked reduction in preload. This contributes to a partial off-loading of the ventricle with a reduction in end-diastolic volume and a decrease in pulmonary capillary wedge pressure (PCWP). At higher doses (i.e, ≥ 150–250 mcg/min) arteriolar dilatation occurs which helps to improve cardiac output through a reduction in afterload and diminished impedance to forward flow.” → https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821770/
Suspension Syndrome
A summary by Alex:
Essentially people get suspended in either mountaineering or industrial accidents and they end up dangling from a harness. When they are rescued they are fine, and then suddenly, usually minutes to days later, they die suddenly. It seems as though people have to be suspended for a few hours for this phenomena to occur.
Here’s the thing, you can read a bunch of papers that confidently assert why this occurs, but no one really knows for sure.
Theories as to why this happens:
1. Volume overload/myocardial rupture- the idea being that you lie them down, and then the blood rushes to the heart and overloads it as there is evidence that mechanical stretch + regional ischemia can cause arrhythmia. BS, these people are hypo or euvolemic, and they really don’t end up with overload, also since these people are more likely to have global hypoxia than local ischemia Pressure needed to actually rupture a healthy (lamb) heart is 526 mmHg. Assuming the person has a healthy heart (no recent MI), than it is very unlikely that one could actually cause this level of pressure to be reached. Hypovolemia requires loss of pretty significant amounts of blood, even at 15% the average healthy person will be pretty much normal. By 30-40% you see serious changes. I guess we can assume that hypervolemia requires similar levels of fluid changes to cause issues on a similar scale.
2. a) Bad blood coming back- immobile legs get hypoxic due to decreased venous return (you need to twitch the small muscles in your legs to avoid this). One theory is that this causes acidosis (which does happen 2 hrs s/p tourniquet a legs venous pH will be 6.9). That said, acidosis transiently decreases cardiac contractility, and really doesn’t cause arrhythmia. It could theoretically cause cariogenic shock, but this seems unlikely as this doesn’t match well with the clinical presentation of suspension syndrome patients.
b) The other side of the “bad blood” argument is potassium leak. This makes more sense and has been seen in crush cases (and the thought is that the physiology is overall pretty similar). That guy had his legs crushed for 8 hours, then had a pH of 7.15 (bad but not awful), and a K of 8 (BAD). He arrested, but they got him back (with what?! bicarb, insulin and glucose which we will discuss later).
So what do you do to treat these people?
In the field: Get access to them, then position them in Fowlers at 30-40 degrees, then slowly lower them to supine. Get ready to treat for complications (EKG, electrolytes, etc). If they have 10+ min of suspension they need to go to an ED. If they have even the most minor signs or symptoms, such as numb legs or transitory respiratory or circulatory problems they need to be admitted on telemetry.
Sources:
- Parker KK, Lavelle JA, Taylor LK, Wang Z, Hansen DE. Stretch-induced ventricular arrhythmias during acute ischemia and reperfusion. J Appl Physiol. 2004; 97:377–383.
- Lyon, Ross T., et al. “Myocardial Rupture: III. Chamber Pressure, Rate of Distention, and Ventricular Disruption in Isolated Hearts.” The Annals of Thoracic Surgery. 1979. doi:10.1016/s0003-4975(10)63369-3.
- Raynovich, Bill. “Dangerous Suspension: Understanding Suspension Syndrome & Prehospital Treatment for Those at Risk.” Journal of Emergency Medical Services. 2009.
- Bishop PA , JB Church: “An alternative mechanism for death by crucifixion.” Linacre Quarterly (J Catholic Medical Assn). 73(3):282Ï289, 2006.
Vocab
Protean (as in “tending or able to change frequently”)
- Schwartz’s Principles of Surgery: “Virtually any organ can become infected, giving rise to the protean manifestations of tuberculosis.”
- Cope’s Early Diagnosis of the Acute Abdomen: “The physician who wishes to be prepared thoroughly to examine and correctly diagnose patients with acute abdominal pain must be fully conversant with these diseases and their protean manifestations.
- Emergency Medicine, Avoiding the Pitfalls and Improving the Outcomes: “Clinical manifestations of SVC syndrome are protean and depend on the degree of vena cava obstruction.”
Step1 Q
A 30 y.o. M is brought to the ED after being the restrained driver in a motor vehicle accident. On physical examination, there is extensive bruising on his chest and abdomen, but no lacerations or open wounds. Blood pressure is 90/55 with a pulse of 122 bpm. On inspiration, his blood pressure is 70/50. On cardiovascular exam, his heart sounds are muffled and he has distended neck veins. What will be a pertinent finding on EKG to support this patient’s diagnosis?
(A) ST elevations in leads II, III, and aVF
(B) Irregularly irregular rhythm without discernible p-waves
(C) QRS complexes that alternate in height
(D) Diffuse ST elevation with PR depression
(E) S wave depth V1 + tallest R wave in V5-V6 > 35 mm
*Pulsus paradoxus
*Beck’s Triad
*Electrical alternans
*Equalization of all chamber pressures –> bad news!
EBM
“BiDil”
- Combo pill for heart failure → isosorbide dinitrate (20mg) and hydralazine (37.5mg)
- First drug approved to treat a general condition in patients of a specific race (and has been criticized as lending credence to the misperception of race as a biological category than social one)
- Approved after 3 trials:
- V-HeFT I → n=459 → no significant difference in all-cause mortality between the treatment group and placebo → post-hoc analysis showed benefit for self-identified African American patients
- V-HeFT II → n=804 → compared BiDil to enalapril → BiDil was found inferior to enalapril → post-hoc analysis showed self-identified racial subgroup (n=215) to have no significant difference (vs inferior for others)
- A-HeFT → n=1050 self-identified black men and women (across 169 US sites) → randomized to receive either BiDil (n=518) or placebo (n=532) for up to 18 months (+ background therapy) → Result was significant efficacy in a composite score of all-cause mortality, first hospitalization for HF, and the Minnesota Living with Heart Failure (MLHF) questionnaire. The drug was associated with a 43% relative reduction in all cause mortality and 8% absolute reduction in first-hospitalizations (16.4% vs. 24.4%).
- NYTimes 2005, Maker of Heart Drug Intended for Blacks Bases Price on Patients’ Wealth → “…set the price of its heart-failure drug BiDil at $1.80 a pill, significantly higher than what analysts had expected and nearly twice as much as some other heart-failure treatments. Depending on the dosage, that would make the cost of taking BiDil at least $5.40 and maybe as much as $10.80 a day.”
One other race based thing to note: even though BiDil was a commercial flop, there are other ways that race is employed in guidelines and modern practice, often perhaps without any better “scientific” backing — that is, maybe it’s just a proxy for something. I would encourage you to always at least question what the role of race is (when you encounter it in guidelines), and look for the science that supports its use. Race is used nowadays in the JNC 8 (2014) and 2017 AHA guidelines, which advise starting hypertensive African American patients on a CCB/thiazide rather than ACEI. We don’t have the space to open that entire can of worms here, but it’s worth noting that all of this relies on the 2002 ALLHAT study. The discussion section of the 2015 study linked below [which is a chart review with “okay” methodology] summarizes the evidence reasonably well.
“Although diuretics or CCBs are recommended as first-line agents in African-American patients, we found no significant difference in the optimal control of blood pressure and frequency of end-organ damage compared to management with other agents.” https://www.ncbi.nlm.nih.gov/pubmed/26713289
— Episode credits —
Hosted by Addie, Kim, and Alex. Audio production and editing by Addie. Show notes written by Addie and Alex.
21 episodes
All episodes
×Welcome to Player FM!
Player FM is scanning the web for high-quality podcasts for you to enjoy right now. It's the best podcast app and works on Android, iPhone, and the web. Signup to sync subscriptions across devices.