Go offline with the Player FM app!
Episode 7: Owning Radiology with Dr. Cliff Tao, Chiropractic Radiologist
Fetch error
Hmmm there seems to be a problem fetching this series right now.
Last successful fetch was on July 01, 2019 13:11 (
What now? This series will be checked again in the next day. If you believe it should be working, please verify the publisher's feed link below is valid and includes actual episode links. You can contact support to request the feed be immediately fetched.
Manage episode 205281689 series 2136888

Episode 7: Owning Radiology with Dr. Cliff Tao, Chiropractic Radiologist
In today’s episode, we talk about utilizing a checklist for each x-ray series you take. We created this form here for your convenience and we hope it really helps to make your practice easy. Download your free Radiology Report Checklist by clicking here.
Use one form per x-ray study and utilize for your Radiology Report just like Dr. Tao discusses in today’s episode.
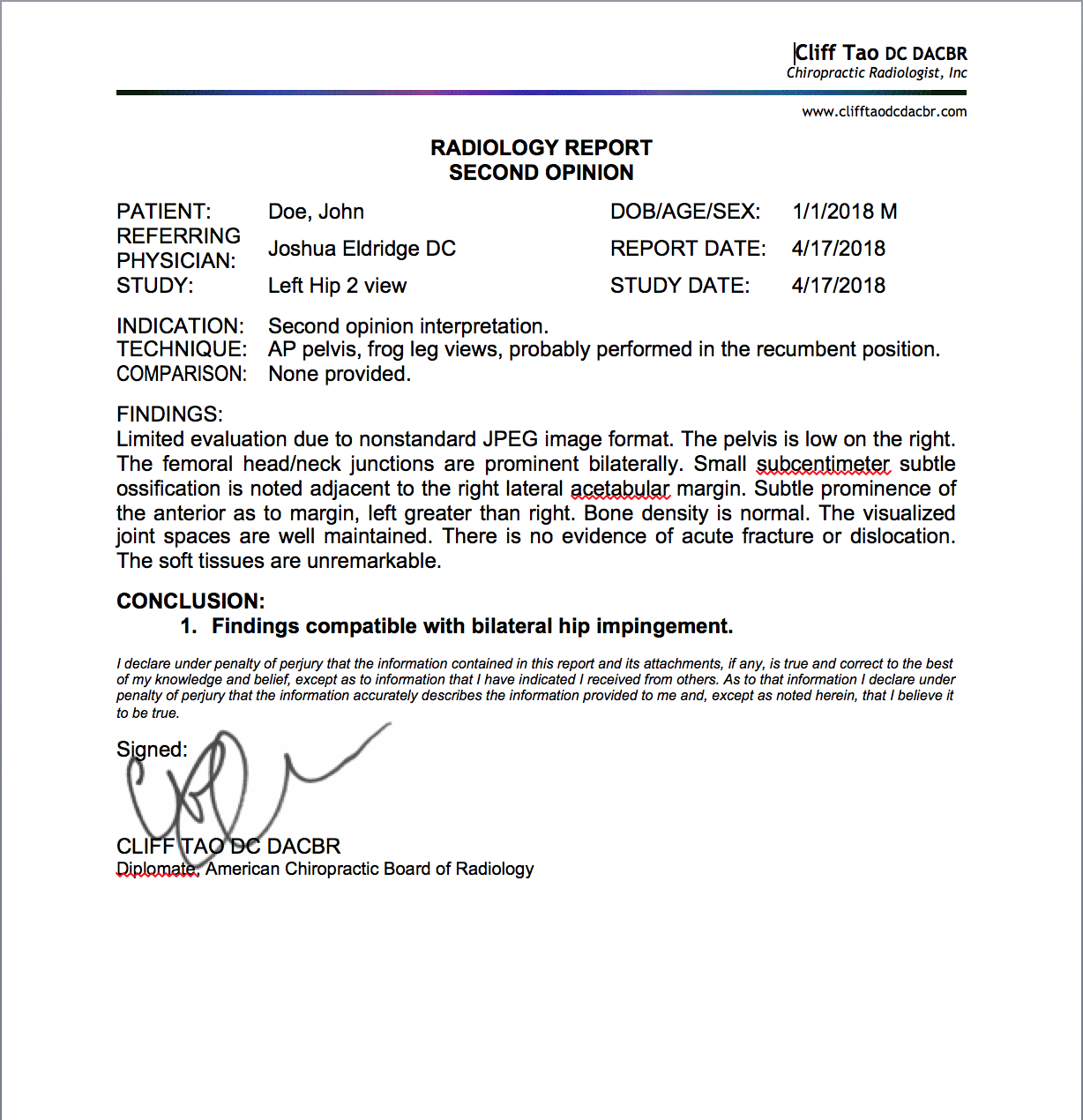
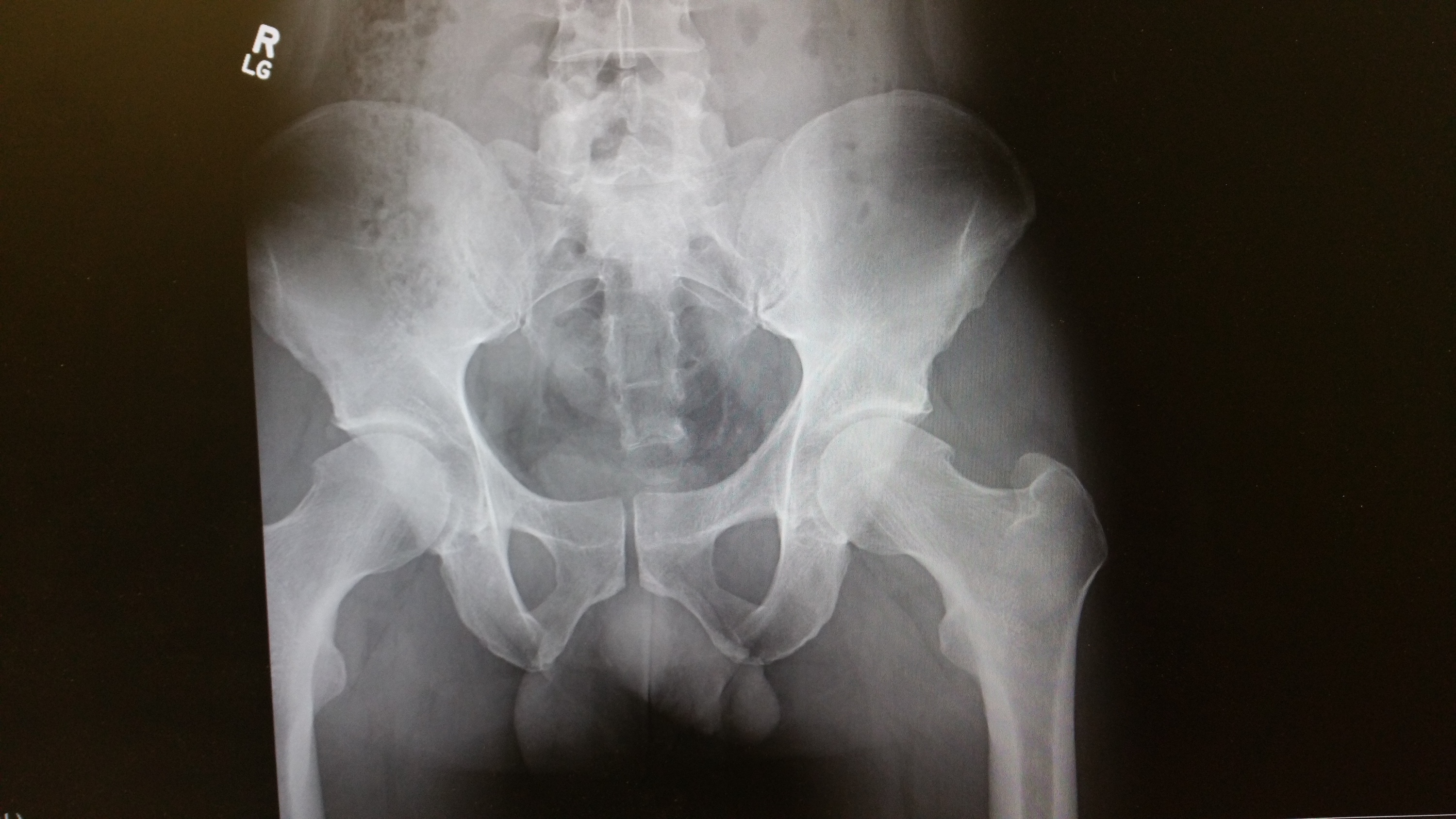
Radiology Report Example
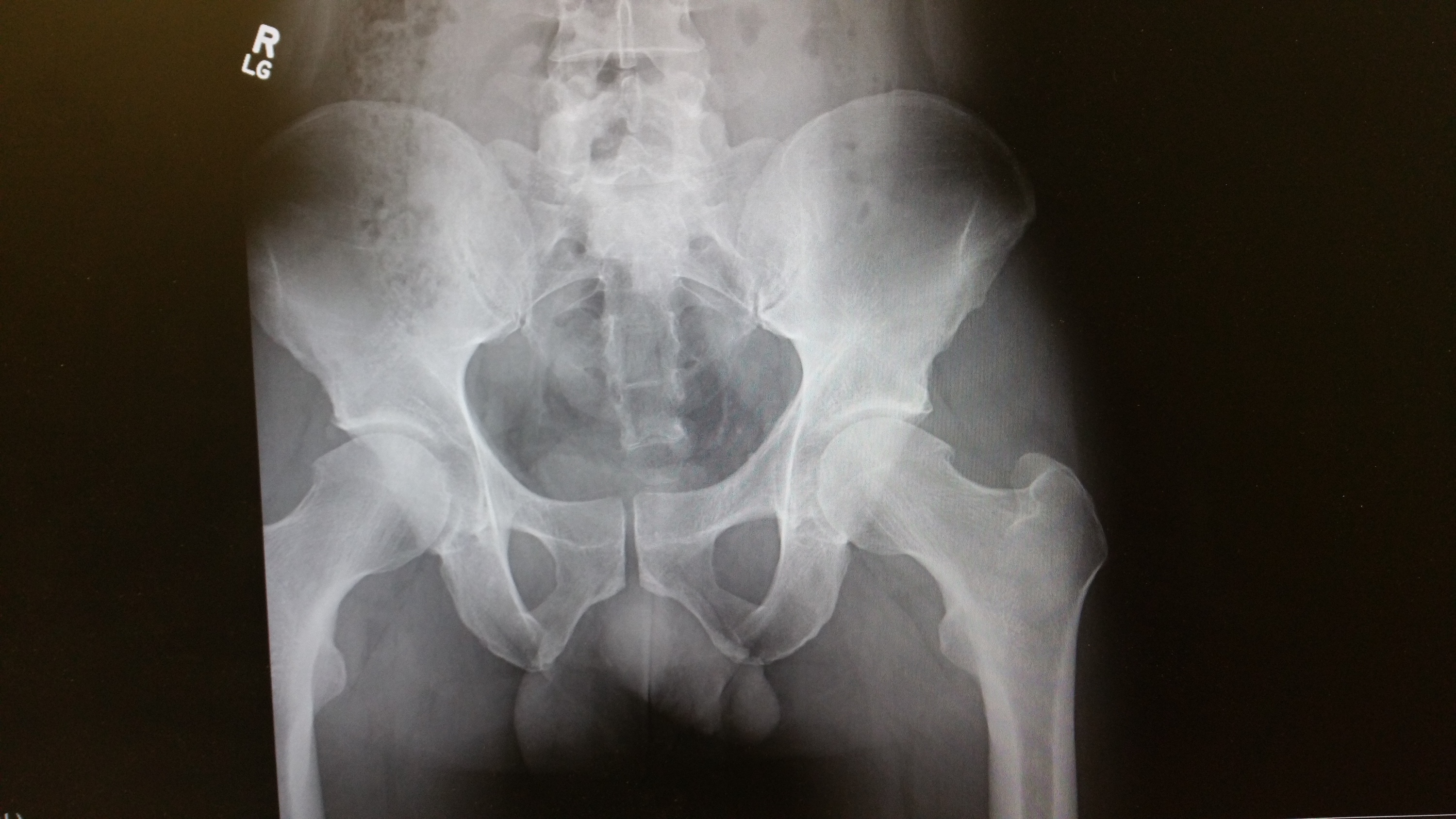
Dr. Tao was gracious enough to share his skills with us and read a hip x-ray for us and composed a report. High quality, precise, and meeting the legal standard just like all of his work. Find out more about Dr. Tao’s services at clifftaodcdacbr.com.
Dr. Joshua Eldridge: Welcome back to episode 7 of the ChiroPractice Pro podcast. On today’s episode, we welcome Dr. Cliff Tao, a chiropractic board-certified radiologist to discuss the most important aspects of reading an X-ray and compiling a proper X-ray report. As our free gift to you, we’ve compiled an X-ray review checklist like Cliff talked about to make sure you review each X-ray you read with accuracy and the special detail your patients deserve. We suggest that you download this checklist and utilize it with every patient. This checklist can also be found in the ChiroPractice Pro system to help you compile a great report every time you use radiology. Also in our show notes, Cliff has presented an X-ray and provided the report for your education.
This is exactly how he does it in his radiology practice. You can see the detail and care he takes with each read. You can find your free X-ray review checklist and the example radiology read in today’s show notes at chiropracticepro.com/episode7. Now, let’s get started with our special guest and my good friend, Dr. Ciff Tao. All right, Cliff, welcome to the ChiroPractice Pro podcast. I’m excited to have you. Just so everyone knows, Cliff and I went to school together back in the dark ages, I think. He got me into radiology. Cliff, welcome to the ChiroPractice Pro podcast.
Dr. Cliff Tao: Thank you, Josh. I didn’t know I got you into radiology, so I apologize.
Dr. Joshua Eldridge: Do you remember? I don’t even if you remember that was so long ago, but we used to go in the mornings to the clinic. That was my favorite part of the day I think.
Dr. Cliff Tao: Oh, okay. Yeah, we did that a few times I think.
Dr. Joshua Eldridge: Yeah, a few hundred maybe. Tell me about your journey becoming a chiropractor and then a radiologist? How did that all work and what got you started? Love to hear about it.
Dr. Cliff Tao: All right, well I suppose I got a short answer and I got a long answer. Short answer is I was in college and I didn’t know what to do afterwards. One of my friends were on a chiropractic school, they got accepted, they’re good friends of mine. They were smart and I’d never even been to a chiropractor, but I checked one out in town. It was actually a little shady, but seemed like a nice guy and I said, well I’m gonna go to chiropractic school. So that’s the short answer.

The long answer is I always had this fascination for the human body. I loved human anatomy especially musculoskeletal anatomy, and my dad is a medical radiologist. Although he didn’t really push me to go into medicine or healthcare, he was more about just do whatever makes you happy kind of guy. My mom was the one that wanted me to either be a doctor or a lawyer. There was that to deal with, but that’s why I went into kinesiology in college, so I could learn a little bit more about musculoskeletal anatomy.
I was involved in sports. I played, I don’t know if you consider it a sport, but I know a lot of people don’t, but I played college badminton all four years. It is a pretty demanding sport. I loved the application of athletics to the human body and how we could optimize the performance. It seemed chiropractic was just a natural segue into it after kinesiology in college. So I got into chiropractic school. Even before I got in, I’d heard that there were specialties in chiropractic, but I thought you had to be really smart or you had to publish stuff to get into these residencies or postdoctoral, postgraduate training types of things. I mean you do have to have some minimal competency, but I don’t think you have to be that smart to do these things. I think you just have to love it, and I love radiology. I love the aspect of having just pictures to look at. Not that I’m not a social person, but I love the aspect where I didn’t have to talk to people all day. I was slightly burned in, this was between college and chiropractic school. I worked at a PI clinic. A motor vehicle accident clinic in Canada.
I saw the business aspect of running a practice. The practice was pretty large. It had five or six locations in the Toronto area in Canada. I liked it from a business perspective, but I didn’t like it from a patient care perspective. That kind of turned me off from having to deal with patients and talk to them and treat them on a regular basis. Radiology was kind of a nice haven for me. I was a little bit away from direct patient care, but I could still have some input into what goes on, maybe not directly but some input into what goes on in the patient management spectrum. Plus, it makes me feel smart. I think you learn a couple extra things in the residency, and the goal really to help patients and help the doctor help the patient, but it gave me a little sense of accomplishment. I’m not that smart. I think I just really liked that aspect of it and the flexibility of working from different locations especially now with digital radiology was also a motivating factor as well. That’s the long story.
Dr. Joshua Eldridge: I don’t want people to think that you’re not smart though, because it takes at least when I remember, to get into the residency to be a DACBR is very difficult and it’s very competitive. I think you’ve done a pretty amazing thing. I have the diplomate in sports, but I think the DACBR might be one step above that. Then us sports guys are just below you in the hierarchy of diplomates.
Dr. Cliff Tao: I’ll go with that, yeah.
Dr. Joshua Eldridge: I think you guys put a lot of work into that. I remember the residence at National as they were preparing to give their boards and how they had to present the cases. That was no joke with questions that they get.
Dr. Cliff Tao: It’s pretty brutal. It’s been a little while for me now. I mean, how long has it been? I finished in 2003, so it’s been about 14 or 15 years, but the residencies were not that organized, so we didn’t even have regular testing and so it really was like a three-year long course and you get one big exam at the end. I remember our cramming session began the week before Christmas. It was 16 weeks of full-time studying, minimal family Christmas time and then the exam was like early April. It’s always like that. I don’t know why they won’t change it. I guess I’ve kind of forgotten about those pains. It was a little difficult, but I think it’s worth it.
Dr. Joshua Eldridge: Yeah, I think you guys have definitely earned it. We were kind of talking offline. I just see the reports that you do compared to similar ones I see from a hospital, I just think they’re so much better. Before we get going into the meat of this, tell me about the most interesting or craziest case you’ve ever seen in radiology? Just off the top of your brain?
Dr. Cliff Tao: Well kind of dovetailing in to what we’re talking offline. One of the craziest cases, I could probably pull up a picture here. You’re not gonna show a picture anyway. Imagine a lateral cervical and there’s no SP’s from C-3 to about C-6. The patient has DISH. Diffuse Idiopathic Skeletal Hyperostosis, and it’s obvious. There’s a big extra bone there anterior to the C-spine. There’s some nuchal bones, so you know, a couple ossifications back there. There’s Degenerative Disc Disease in the osteophytes that you’d normally expect from, I don’t remember how old the patient was, but probably in their 50’s or 60’s. This was a patient that went to a local hospital to get X-rays for some reason. The report came back from the medical radiologist. It was one line long, and it said multilevel degenerative disease, period, and that was it.
Radiologically, it’s an easy diagnosis to make. Maybe from a medical standpoint, it doesn’t matter to them but as chiropractors, we’re gonna be palpating the SP’s and a laminin, stuff like that. We kind of need to know if those things are there or not. That’s a case I put in my presentation that I do regularly for CE and stuff like that. I always kind of say just because you sent your patient out for X-rays to professionals, I encourage everyone to at least look at the images and not to just rely on the report that you get.
Dr. Joshua Eldridge: For sure. Getting into this. When we think about imaging, what should be the first thing that comes to mind before we make the clinical decision that imaging is necessary? When we make that decision when we’re in the room and we’re working with a patient, what should be our thought process before we image the patient?
Dr. Cliff Tao: I don’t really get into that a lot. Part of the reason is I service a lot of different chiropractors. As you know, on one end of the spectrum, we have a very mainstream medically oriented chiropractors that just function like a medical physician, and then on the other end of things, I have my vitalistic or philosophically-oriented subluxation-based chiropractors who don’t have such strict criteria when deciding whether or not to order X-rays or other imaging.
Just as a very broad generalization, I’ll say if you feel like having an X-ray is gonna help you treat the patient better, get the patient better, then go ahead, take the X-ray, or order the X-ray. I’m a little liberal in that sense. I don’t really follow the published guidelines or recommendations or anything like that. It’s probably not great. Sorry, I’m a little liberal in that case. I don’t care, or not that I don’t care, but it doesn’t matter to me what particular technique you use or how you treat them. I don’t know what’s out there. I’m kind of removed from that process. I just assume the chiropractor that I’m serving knows what he or she is doing and knows when it’s gonna be a good idea to take X-rays or not.
Dr. Joshua Eldridge: All right, do you have any practice guidelines that you suggest to different practitioners if they ask? Is that something that you’ve looked at or not as much just because you’re more removed from that?
Dr. Cliff Tao: Yeah, not as much. I try not to get into it. It seems like we almost need two sets of guidelines for the two opposite ends of our spectrum. On one end, we have the ACA, choose wisely which I think that recommendation was made without any radiologist consultation, so there’s that as well. Then we have the other and the spectrum, they have a set of guidelines too which of course are a little more liberal and a little more open-ended. I don’t really recommend either one, I guess if I were to, it would just be dependent on what type of practice this particular chiropractor has.
Dr. Joshua Eldridge: I know in the hospital setting, they really don’t want us to do especially the lumbar spine X-rays. It’s something that they really push for us not to do unless there’s trauma or there’s some type of neurological deficit that we find in the exam, or trauma, neurological deficit or something that clinically we think that there’s an injury that’s occurred or some type of disease process going on that could potentially be causing the symptoms of the patient. And they have guidelines that say if you have a certain percentage, if you ordered let’s say 25%, then you’ve exceeded the guidelines and therefore should be looked at closer. Yeah, it’s a different situation because you’ve got a lot of accountants in the next two. There’s a lot of studies out there that say once you have the X-ray, is it gonna change your potential treatment. I guess that gets back into our job as more clinicians to decide that, and then just a thought.
Dr. Cliff Tao: Part of the problem I think is that, I don’t know when it started, probably early 1900’s when they discovered that radiation was not that great for the body. We still hold on to that, and there’s still truth to that, but I think a lot of those studies have proved radiation was bad for high levels of radiation or even moderate levels of radiation. That we know is bad. I’m talking like the recent was at Fukushima, the nuclear plant in Japan. That’s super high amounts of radiation, but there’s been a lot of data that show what low levels amount of radiation will do. Low-level meaning from X-ray, CT scans.
When you have no data, you can only really guess. I don’t know if it’s good, if it’s bad or if there’s no effect. I still think there should be some caution involved or let’s just be conservative and say hey let’s not just blast everybody with X-rays because we don’t know what it’s doing, could be good, could be bad, it could have no effect, but there should be some clinical or critical thinking involved before you plan to take an X-ray.
Dr. Joshua Eldridge: I like that. That’s a good way to leave that one. I think that’s a good way to go. So just be smart. Once we’ve taken the X-ray, how do we make sure we’re not missing anything? So you got the X-ray, let’s just say a lumbar spine. We got a lumbar spine X-ray and it’s up here in front of us, either on our monitor or on the viewer, what process do we have to go through to make sure that as clinicians, we don’t miss anything?
Dr. Cliff Tao: Well, I think it’s a good idea to have a checklist. The longer the checklist, the more thorough you are. I think everybody learned what I learned in school and what I learned in residency too were the ABCS, and that goes for spine and most other bone or musculoskeletal types of X-rays. Everybody knows A is for alignment, B for bone, C is for cartilage or joint spaces, and S is for soft tissues. That’s a good place to start, but then we have to realize there’s a little more under each letter. We could go further into it.
Dr. Joshua Eldridge: Go for it. Tell us about alignment.
Dr. Cliff Tao: Alignment, that’s probably the easiest one. Just making sure the bones line up on each view and then that’s kind of the reason why we got to have the right views first of all, and everyone knows this again, you got to have an AP and a lateral. Earlier before we started, I was saying I had a pediatric ankle fracture. I’ve seen a few of these where the fracture only shows up on one view especially in the ankle. It must be that it’s just more common, but I think it showed up on the lateral view, not on the A to P and not on the oblique view even. We got to have at least two or maybe even three more views to have a more thorough assessment. Alignment is make sure all the bones line up. B of course for bone and naturally, we think of bone density to start with.
That in itself is as hard to evaluate because the X-ray is not really for looking at bone density, it’s more looking at the anatomy. We know we need at least 30% to 50% loss of bone density in order for us just to identify it on X-ray. It’s worse in the spine by the way, so that number 30% to 50% is average for all the bones in the body, but in the spine and in particular, the lumbar spine, I think that number’s 70% to 80%, so it’s actually pretty bad in the lumbar spine. We have to kind of keep that in the back of our mind. The other things that are under B are the shape of the bone, it’s the shape or the morphology of the bone, and does that look okay. Are there little osteophytes here and there, are there erosions, is there sclerosis for example when describing a fracture.
This is more important if you’re communicating with the orthopedist or someone who’s in between the fracturing or they want to know the prognosis of the fracture. How close are the ends? Are they opposed, is there displacement, angulation, rotation? Is there a fragmentation? All these things are covered under B and in this specific example under if there’s a fracture. C is for cartilage or soft joint spaces. So you just think of for example, in the spine, the disc, there’s cartilaginous end plate or the annular fibers and then there’s the nucleus pulposus. You gotta look at those things, although we can’t really see them, but there’s ossification or calcification with them, we can comment on it as indirect relation to what we know is there.
Of course, the disc spaces can be increased or decreased, of course, most commonly, they’re gonna be decreased much more commonly than increased. Then is there abnormal change in the joint space? So in the spine, is there a wedging one way or the other, laterally, medially, what-have-you. There’s other areas where there’s cartilage too. So the other joints, so like the hip joints and the lumbar spine, or the symphysis pubis, all those joints that have cartilage that really look like spaces, but they’re not. Then S, I feel like a lot of people just gloss over the S because we really don’t see soft tissues that well on an X-ray, but on a well exposed or X-ray that’s done with good technique, you can see quite a bit of soft tissues and you can get a lot of information from them.
But we do of course have to realize that there’s a lot of stuff we don’t see on X-ray and there’s other stuff that we can use to evaluate the soft tissues, like a CT scan, ultrasound or an MRI, but just don’t forget to look at the soft tissues. Note any for example, common ones, atherosclerosis which everyone has seen in the abdominal aorta, but you can get that in the carotid sinuses in the neck, you can get in the upper vertebral arteries, you can get it in the ankle and the wrist which could indicate diabetes. That’s common in the soft tissue realm. How’s that?
Dr. Joshua Eldridge: That’s good, and swelling too, maybe soft tissue? Did you hit that one?
Dr. Cliff Tao: No, I didn’t mention it, but yeah that’s a good one too. Hard to see that directly, but easy to miss if you don’t look for it, but yeah we see that not infrequently for example in the knee, suprapatellar swelling or in the anterior wrist. Lot of times it’s just there’s a fat pad that looks a little deviated, some type of an indirect assessment of that.
Dr. Joshua Eldridge: That’s really good, and I think that that’s a good review because people forget and they’re just out there looking at X-rays and they’re looking if they do Gonstead, they’re just drawn on it for their manipulations or whatever they’re doing, and then they forget about all the important stuff that might be in there as well. I like the checklist idea. That’s just like a pilot where people’s lives are a little bit more important, but making sure you go through that each time. Cliff, get into the how you write a report then. We’ve gone through the ABCS, and get into how you write a report on that? What’s the different components to report, what should be on there legally. From a legal standard, what do you need to have?
Dr. Cliff Tao: Well, I think everyone knows this, but you gotta have the patient information at the get-go. So, patient name, date of birth, their gender, the date of the X-ray and of course, a date that you’re doing your report. I like to have a little bit of clinical indication in there, why you took the X-ray or maybe there’s something on the X-ray that looks a little funky to you. Also, sometimes, I like to put where the X-ray was taken if I know it’s not taken at the doctor’s office. In med-legal cases, sometimes it matters I think where the X-ray was done. For example, if the X-ray study was not great quality, who do you blame? The chiropractor or do you blame the Imaging Center? I think that matters too. Then you get into the meat of the X-ray report. Basically, there’s two sections in the meat, so there’s the findings section and there’s the impression or conclusion.
In the findings section, generally speaking, this is just what we see. It’s kind of the nitty-gritty, do I see a white thing, do I see a dark thing, was it round, was it square? Is it pointy? That’s where you go to town on describing what you see. Actually even before we get there, or right before we get there, I like to look at X-rays twice. I think the first time you look at an X-ray should be without any biased information. You just kind of forget about what the patient is in for, whether they have pain or not, if you can forget about what they look like. All that stuff is all extra information to me. Just look at the image for what it is, just the image and that will force you to be a little more objective, I think, and it’ll force you to look at the whole image which you should be looking at anyway. Then, you got to kind of reinsert that information back in your brain, Oh, okay. They came in because they’ve had back pain for three years, and they fell 10 years ago or whatever.
That should kind of focus you into a particular area and maybe it’ll change your report, maybe it won’t. A lot of times, it does. It takes a little bit longer I think to read an X-ray that way, but I think it’s a little more thorough and a little more objective that way. I do that and then you write it down, the nitty-gritty, what you see in the findings section. Then in the impression or the conclusions, that’s what you think of the findings. It’s what you think of what you just saw. Are they all normal things that you just saw, or is it degenerative disease? Is it spondylosis? Is it a fracture? And then kind of a subset of the conclusion or impression section is at least for me, recommendations. Are there further things you can do to figure this out? Do you need to take another X-ray view? Do you need to take the other side, or you need to get a CT scan or something? That’s where all that information goes. Then, of course, you have to sign the report at the end and I think that’s it.
Dr. Joshua Eldridge: All right, nice. Then once you’re done with everything, how do you build it back into your clinical relevance with the patient? I know as a radiologist, you’re just kind of sending it back and you’re giving your two cents on it, but then what about if it’s your patient? How do you kind of build that all back into your treatment plan, and how do you present it to the patient?
Dr. Cliff Tao: Well, I think you can do it a few different ways. One way is just to kind of show your patient the report. I think it probably depends on what’s on the report and what or how you perceive your patient to be. Do you really need to have your patients know every little detail about their X-rays, and is it gonna make that much of a difference? Those are things I think can be determined on a case-by-case basis. This is not a familiar scenario to me, so I think if it was me, I would wanna know. It takes more time obviously for the doc to kind of go through all these findings and hopefully they can sort out what’s relevant and what’s not relevant, and hopefully, the patient will have a little more confidence in treatment plan that the doctor’s proposing. Generally speaking, I use it to either refute or confirm your suspicions before the X-ray and maybe it’ll help you support your proposed treatment plan or management plan for the patient.
Dr. Joshua Eldridge: I know that for me, whenever I have radiology on the patient, let’s say lumbar spine, or there’s some spondylosis on there, and I’m able to say that’ll change my diagnosis code from something like lower back pain to actual spondylosis. Now it also increases your medical decision making like we talked about in podcast 2 and 3 with Warren Jahn, but that’s part of your assessment too. It’s gonna increase your medical decision making that you’ve looked at this X-ray and now you’re giving them a diagnosis of spondylosis or spondylosis with radiculopathy. It changes that hierarchy of your diagnosis codes. That’s a big deal when you’re talking about reimbursement because you wanna make sure that you get paid for what you’re doing. If someone brings in their X-rays from a previous chiropractor and they were more let’s say, subluxation based and you took the time to read through the X-rays, and you see that there’s something abnormal that might be something as well to justify your treating the patient to a third party as well.
Dr. Cliff Tao: Right, of course.
Dr. Joshua Eldridge: Tell me about your services that you provide. How does that work? When I’m in my office and I take an X-ray, how does Dr. cliff get my information to read my X-rays?
Dr. Cliff Tao: Well, it’s not that complicated. In my typical chiro that I serve, they have an X-ray in their office, they’re digital X-rays. There are several ways of getting the digital X-rays to me, so we set that up. It could be as easy as, soon as the X-ray is done on their end, they’re done taking the X-rays, they might have to hit one or two buttons and the X-ray gets sent over to me. It shows up on my computer within about 5 to 10 minutes, and I see it immediately. I can do it right away. Typically it takes us, meaning I also have a few associates here, or not here, but out there. It takes us about 24 to 48 hours to generate a formal report and get it back to you.
Actually, some of my guys have it set up where they just want a more routine process. I think they have a higher volume maybe of X-rays so it’s worth it to them. They have it set up, so it actually doesn’t take them anytime to send me the X-ray. The computer knows as soon as the study is done, it gets automatically sent to me. That way, they don’t spend any time trying to figure out how to send the X-ray to me when to send it, which studies to send, it just gets done automatically. I have a few guys like that as well. Most of my guys are, they send on just a case by case basis. They see something weird, they’ll send it to me, or if it’s maybe a complex case, then they don’t get it. But it’s not that hard. Once you get it going, it’s an easy process to send the study over.
Dr. Joshua Eldridge: Why would me as a chiropractor serving my city or my tribe here, why would I wanna send you my X-rays? What is the benefit to having a specialist look at my X-rays?
Dr. Cliff Tao: Well, I mean you could look at it a few different ways. I think it’s better, you get a more accurate report off of the X-rays. I’m probably thinking more of an idealistic situation. If it was your eye and we went to just a medical doctor and they took X-rays in our office, when you want a specialist look at your X-rays rather than– We’re all trained to read X-rays, but I just happen to have a little more training and it’s what I do all day. I think it just gives a higher level of service and professionalism to your practice. It could help streamline things too. I think it’s hard when chiropractors in a busy practice, they’re taking X-rays and they’re reading them. You might read a lot of X-rays, but I’ll tell you, there’s a lot of different things that I see on X-rays and that I don’t see on X-rays that chiropractors don’t see, or do see and then I don’t see them.
There’s over calls, there’s under calls. I’m talking ideal practice here, but we would like to try to minimize false negatives and minimize false positives. Then there’s special cases like med-legal cases. I think it always helps to get another chiropractor or another healthcare practitioner on the case. It just helps kind of spread the liability. I hate to say it, but it does spread the liability a little bit, but it also shows that we know what our limits are. When it comes to complicated X-ray that you have someone to send it to and do a more thorough job looking at it.
Dr. Joshua Eldridge: Alright, that sounds good. I know you do a case online, you put a few up on Facebook every now and then and people should definitely check that out. What are the percentage in your experience that chiropractors that are doing their own X-rays are missing things? And use me for an example. I don’t mind. I got broad shoulders, so I can take it. But if I got 10 X-rays, how many of those am I missing something on?
Dr. Cliff Tao: Oh, you know it’s very variable. I hate to say this, but for you, you probably wouldn’t miss a whole lot. It’d be probably less than one. Actually, it’d be probably more than one, but of the things that you miss, then you gotta look at does it really make a difference? Okay, so you missed a little osteophyte at L-1. Is that gonna make a difference? Probably not in your practice, but it might make a difference in someone else’s practice, so it’s hard to say. I do have some chiros that I think seem to miss on every single X-ray. I’m not gonna give any names, but I we’re all over the map.
There’s some guys that do very well at reading X-rays, but they send me all their X-rays because they kind of know that there’s a lot of stuff that goes on that they don’t really see if they’re not trained or reading them on a regular basis. Then I have guys that send me stuff but almost on every image, I gotta make a special call to them or special email to them to make sure they saw something. Those happen frequently. I don’t really know exactly how it impacts the patient in the end, but I’d say at least maybe on average, maybe 20% would have a significant impact on how you’re gonna treat the patient.
Dr. Joshua Eldridge: To me, that’s a big deal. 20%’s a big deal when it comes to treating a patient. That’s a lot to miss. Of those 20%, some of that could be like we just talked about in osteoma in the skull.
Dr. Cliff Tao: Yeah.
Dr. Joshua Eldridge: If you missed something like that, that could be the patient’s life at some point.
Dr. Cliff Tao: Right, yeah. It’s not a best-case scenario that the chiropractor would be adequately trained to read all imaging, but it’s hard to be good in everything. There’s some guys out there that they’re really good with all that stuff, but I tell a lot of my chiros, hey, I don’t talk to your patients. You should be looking at the X-rays that you take, but maybe from a preliminary standpoint, and then you send it to me. You and I can talk about it but in the end, I should be doing that final analysis or final report on the X-rays. I hate to bring this into it, but from a med-legal standpoint, if you ever get subpoenaed for your records or whatever and you’re the last, why didn’t you just send this to a radiologist to read? There’s rarely a good answer for that, at least that I’ve seen. I think it’s good in the end. I know I’m kind of talking from an idealistic standpoint, but from a perfect scenario, we’d have a specialist doing everything, but we’re not in a perfect world.
Dr. Joshua Eldridge: Right, so if people wanna find out more about your services, where do they go to find out more about your services? How can they get ahold of you?
Dr. Cliff Tao: Oh, well they can go to my website. Should I give you the website?
Dr. Joshua Eldridge: Yeah, go for it.
Dr. Cliff Tao: Okay, it’s www.clifftaodcdacbr.com.
Dr. Joshua Eldridge: Tao is T-A-O. Just so people know that. C-L-I-F-F T-A-O.
Dr. Cliff Tao: Yes, same thing on Facebook. I’m pretty active on Facebook so you could search me with Cliff Tao, DC DACBR, and same thing on LinkedIn as well, or they can call me, 714-876-1126. I might not pick up the phone, but at least you can call me, and I’ll call you back eventually.
Dr. Joshua Eldridge: Now, the other cool thing that you do, you do a really cool event that just happened last weekend. It’s an amazing ski trip that you do up at Mammoth Mountain each year. Tell us a little bit about what you do and what kind of time it is for those chiros that come out there.
Dr. Cliff Tao: Alright, we’ve been doing it for about seven years now, just had it last weekend. It’s always at Mammoth Mountain. Obviously, Josh, I love to ski. That’s one of my passions, but so is chiropractic. They say you should work smarter, not harder so I’ve combined two of my passions for a two-in-one weekend where you can get continuing education and some great skiing in. What I do, I bring in a few speakers that I know, that do a good job. It’s kind of a mishmash all over the place. This past year, we had a great guy talking about documentation, another guy talking about personal injury, another guy talking about pediatric adjusting and a neurology guy, a neuro diplomate talking about his neuro exam and stuff like that. It’s kind of different guys and gals talking about their specialty within chiropractic. I try to keep it pretty formal on the CE, or not formal, but we’re dressed very informally because we’ve just gotten off the ski lifts or something, but we do have food there. It’s generally a pretty good time.
Dr. Joshua Eldridge: That’s pretty cool. They find more information about that at your website as well?
Dr. Cliff Tao: That’s on my website as well, yeah.
Dr. Joshua Eldridge: Perfect. That’s something that I am very much looking forward to. I really wanna come out this next year and come to your event and hang out. The last time me and you skied together was in Michigan when you broke your fibula.
Dr. Cliff Tao: Yes, boot top fracture.
Dr. Joshua Eldridge: Yeah, I remember that one.
Dr. Cliff Tao: I had no insurance by the way.
Dr. Joshua Eldridge: Back in the day, huh?
Dr. Cliff Tao: Yes, I have insurance now.
Dr. Joshua Eldridge: Just in case it happens. Are you still doing the crazy stuff down the slopestyle? Are you coming down and hit the tabletops and all that kind of stuff?
Dr. Cliff Tao: No, I don’t do those anymore, Josh. I’m a little too risky now, and I’m a little more fragile now. I stay off those things. I do get a little bit of air, but not much air these days. Yeah, I would love to have you come out and it’d be a great time. Yes, it’s fun times. A nice little venue and just a small group of guys. Usually, we have about 20 people, probably a little more next year maybe, but good skiing and you can learn a couple things, and hopefully get some CE in there too.
Dr. Joshua Eldridge: Nice, well, Cliff, thanks for joining us on the ChiroPractice Pro podcast. I really enjoyed having you, and thanks for taking the time and sharing your knowledge about radiology.
Dr. Cliff Tao: You’re very welcome, Josh. Thanks for having me.
Dr. Joshua Eldridge: All right, you bet. Thank You, Cliff, for joining us on the ChiroPractice Pro podcast. Don’t forget to download your free X-ray review checklist and see the example X-ray read at chiropracticepro.com/episode7. We enjoyed having you on today’s episode, and we hope that you found real value with the podcast. If the ChiroPractice Pro podcast has helped you in your practice, take a moment and leave a review on iTunes and then share with another chiropractor that you respect. From our team here at ChiroPractice Pro, we want to say thank you in advance for doing this. Don’t forget that to be successful in practice, it’s all about the little things. Keep doing the little things each day to see big results. We’ll see you next time right here at chiropracticepro.com.
11 episodes
Fetch error
Hmmm there seems to be a problem fetching this series right now.
Last successful fetch was on July 01, 2019 13:11 (
What now? This series will be checked again in the next day. If you believe it should be working, please verify the publisher's feed link below is valid and includes actual episode links. You can contact support to request the feed be immediately fetched.
Manage episode 205281689 series 2136888

Episode 7: Owning Radiology with Dr. Cliff Tao, Chiropractic Radiologist
In today’s episode, we talk about utilizing a checklist for each x-ray series you take. We created this form here for your convenience and we hope it really helps to make your practice easy. Download your free Radiology Report Checklist by clicking here.
Use one form per x-ray study and utilize for your Radiology Report just like Dr. Tao discusses in today’s episode.
Radiology Report Example
Dr. Tao was gracious enough to share his skills with us and read a hip x-ray for us and composed a report. High quality, precise, and meeting the legal standard just like all of his work. Find out more about Dr. Tao’s services at clifftaodcdacbr.com.
Dr. Joshua Eldridge: Welcome back to episode 7 of the ChiroPractice Pro podcast. On today’s episode, we welcome Dr. Cliff Tao, a chiropractic board-certified radiologist to discuss the most important aspects of reading an X-ray and compiling a proper X-ray report. As our free gift to you, we’ve compiled an X-ray review checklist like Cliff talked about to make sure you review each X-ray you read with accuracy and the special detail your patients deserve. We suggest that you download this checklist and utilize it with every patient. This checklist can also be found in the ChiroPractice Pro system to help you compile a great report every time you use radiology. Also in our show notes, Cliff has presented an X-ray and provided the report for your education.
This is exactly how he does it in his radiology practice. You can see the detail and care he takes with each read. You can find your free X-ray review checklist and the example radiology read in today’s show notes at chiropracticepro.com/episode7. Now, let’s get started with our special guest and my good friend, Dr. Ciff Tao. All right, Cliff, welcome to the ChiroPractice Pro podcast. I’m excited to have you. Just so everyone knows, Cliff and I went to school together back in the dark ages, I think. He got me into radiology. Cliff, welcome to the ChiroPractice Pro podcast.
Dr. Cliff Tao: Thank you, Josh. I didn’t know I got you into radiology, so I apologize.
Dr. Joshua Eldridge: Do you remember? I don’t even if you remember that was so long ago, but we used to go in the mornings to the clinic. That was my favorite part of the day I think.
Dr. Cliff Tao: Oh, okay. Yeah, we did that a few times I think.
Dr. Joshua Eldridge: Yeah, a few hundred maybe. Tell me about your journey becoming a chiropractor and then a radiologist? How did that all work and what got you started? Love to hear about it.
Dr. Cliff Tao: All right, well I suppose I got a short answer and I got a long answer. Short answer is I was in college and I didn’t know what to do afterwards. One of my friends were on a chiropractic school, they got accepted, they’re good friends of mine. They were smart and I’d never even been to a chiropractor, but I checked one out in town. It was actually a little shady, but seemed like a nice guy and I said, well I’m gonna go to chiropractic school. So that’s the short answer.

The long answer is I always had this fascination for the human body. I loved human anatomy especially musculoskeletal anatomy, and my dad is a medical radiologist. Although he didn’t really push me to go into medicine or healthcare, he was more about just do whatever makes you happy kind of guy. My mom was the one that wanted me to either be a doctor or a lawyer. There was that to deal with, but that’s why I went into kinesiology in college, so I could learn a little bit more about musculoskeletal anatomy.
I was involved in sports. I played, I don’t know if you consider it a sport, but I know a lot of people don’t, but I played college badminton all four years. It is a pretty demanding sport. I loved the application of athletics to the human body and how we could optimize the performance. It seemed chiropractic was just a natural segue into it after kinesiology in college. So I got into chiropractic school. Even before I got in, I’d heard that there were specialties in chiropractic, but I thought you had to be really smart or you had to publish stuff to get into these residencies or postdoctoral, postgraduate training types of things. I mean you do have to have some minimal competency, but I don’t think you have to be that smart to do these things. I think you just have to love it, and I love radiology. I love the aspect of having just pictures to look at. Not that I’m not a social person, but I love the aspect where I didn’t have to talk to people all day. I was slightly burned in, this was between college and chiropractic school. I worked at a PI clinic. A motor vehicle accident clinic in Canada.
I saw the business aspect of running a practice. The practice was pretty large. It had five or six locations in the Toronto area in Canada. I liked it from a business perspective, but I didn’t like it from a patient care perspective. That kind of turned me off from having to deal with patients and talk to them and treat them on a regular basis. Radiology was kind of a nice haven for me. I was a little bit away from direct patient care, but I could still have some input into what goes on, maybe not directly but some input into what goes on in the patient management spectrum. Plus, it makes me feel smart. I think you learn a couple extra things in the residency, and the goal really to help patients and help the doctor help the patient, but it gave me a little sense of accomplishment. I’m not that smart. I think I just really liked that aspect of it and the flexibility of working from different locations especially now with digital radiology was also a motivating factor as well. That’s the long story.
Dr. Joshua Eldridge: I don’t want people to think that you’re not smart though, because it takes at least when I remember, to get into the residency to be a DACBR is very difficult and it’s very competitive. I think you’ve done a pretty amazing thing. I have the diplomate in sports, but I think the DACBR might be one step above that. Then us sports guys are just below you in the hierarchy of diplomates.
Dr. Cliff Tao: I’ll go with that, yeah.
Dr. Joshua Eldridge: I think you guys put a lot of work into that. I remember the residence at National as they were preparing to give their boards and how they had to present the cases. That was no joke with questions that they get.
Dr. Cliff Tao: It’s pretty brutal. It’s been a little while for me now. I mean, how long has it been? I finished in 2003, so it’s been about 14 or 15 years, but the residencies were not that organized, so we didn’t even have regular testing and so it really was like a three-year long course and you get one big exam at the end. I remember our cramming session began the week before Christmas. It was 16 weeks of full-time studying, minimal family Christmas time and then the exam was like early April. It’s always like that. I don’t know why they won’t change it. I guess I’ve kind of forgotten about those pains. It was a little difficult, but I think it’s worth it.
Dr. Joshua Eldridge: Yeah, I think you guys have definitely earned it. We were kind of talking offline. I just see the reports that you do compared to similar ones I see from a hospital, I just think they’re so much better. Before we get going into the meat of this, tell me about the most interesting or craziest case you’ve ever seen in radiology? Just off the top of your brain?
Dr. Cliff Tao: Well kind of dovetailing in to what we’re talking offline. One of the craziest cases, I could probably pull up a picture here. You’re not gonna show a picture anyway. Imagine a lateral cervical and there’s no SP’s from C-3 to about C-6. The patient has DISH. Diffuse Idiopathic Skeletal Hyperostosis, and it’s obvious. There’s a big extra bone there anterior to the C-spine. There’s some nuchal bones, so you know, a couple ossifications back there. There’s Degenerative Disc Disease in the osteophytes that you’d normally expect from, I don’t remember how old the patient was, but probably in their 50’s or 60’s. This was a patient that went to a local hospital to get X-rays for some reason. The report came back from the medical radiologist. It was one line long, and it said multilevel degenerative disease, period, and that was it.
Radiologically, it’s an easy diagnosis to make. Maybe from a medical standpoint, it doesn’t matter to them but as chiropractors, we’re gonna be palpating the SP’s and a laminin, stuff like that. We kind of need to know if those things are there or not. That’s a case I put in my presentation that I do regularly for CE and stuff like that. I always kind of say just because you sent your patient out for X-rays to professionals, I encourage everyone to at least look at the images and not to just rely on the report that you get.
Dr. Joshua Eldridge: For sure. Getting into this. When we think about imaging, what should be the first thing that comes to mind before we make the clinical decision that imaging is necessary? When we make that decision when we’re in the room and we’re working with a patient, what should be our thought process before we image the patient?
Dr. Cliff Tao: I don’t really get into that a lot. Part of the reason is I service a lot of different chiropractors. As you know, on one end of the spectrum, we have a very mainstream medically oriented chiropractors that just function like a medical physician, and then on the other end of things, I have my vitalistic or philosophically-oriented subluxation-based chiropractors who don’t have such strict criteria when deciding whether or not to order X-rays or other imaging.
Just as a very broad generalization, I’ll say if you feel like having an X-ray is gonna help you treat the patient better, get the patient better, then go ahead, take the X-ray, or order the X-ray. I’m a little liberal in that sense. I don’t really follow the published guidelines or recommendations or anything like that. It’s probably not great. Sorry, I’m a little liberal in that case. I don’t care, or not that I don’t care, but it doesn’t matter to me what particular technique you use or how you treat them. I don’t know what’s out there. I’m kind of removed from that process. I just assume the chiropractor that I’m serving knows what he or she is doing and knows when it’s gonna be a good idea to take X-rays or not.
Dr. Joshua Eldridge: All right, do you have any practice guidelines that you suggest to different practitioners if they ask? Is that something that you’ve looked at or not as much just because you’re more removed from that?
Dr. Cliff Tao: Yeah, not as much. I try not to get into it. It seems like we almost need two sets of guidelines for the two opposite ends of our spectrum. On one end, we have the ACA, choose wisely which I think that recommendation was made without any radiologist consultation, so there’s that as well. Then we have the other and the spectrum, they have a set of guidelines too which of course are a little more liberal and a little more open-ended. I don’t really recommend either one, I guess if I were to, it would just be dependent on what type of practice this particular chiropractor has.
Dr. Joshua Eldridge: I know in the hospital setting, they really don’t want us to do especially the lumbar spine X-rays. It’s something that they really push for us not to do unless there’s trauma or there’s some type of neurological deficit that we find in the exam, or trauma, neurological deficit or something that clinically we think that there’s an injury that’s occurred or some type of disease process going on that could potentially be causing the symptoms of the patient. And they have guidelines that say if you have a certain percentage, if you ordered let’s say 25%, then you’ve exceeded the guidelines and therefore should be looked at closer. Yeah, it’s a different situation because you’ve got a lot of accountants in the next two. There’s a lot of studies out there that say once you have the X-ray, is it gonna change your potential treatment. I guess that gets back into our job as more clinicians to decide that, and then just a thought.
Dr. Cliff Tao: Part of the problem I think is that, I don’t know when it started, probably early 1900’s when they discovered that radiation was not that great for the body. We still hold on to that, and there’s still truth to that, but I think a lot of those studies have proved radiation was bad for high levels of radiation or even moderate levels of radiation. That we know is bad. I’m talking like the recent was at Fukushima, the nuclear plant in Japan. That’s super high amounts of radiation, but there’s been a lot of data that show what low levels amount of radiation will do. Low-level meaning from X-ray, CT scans.
When you have no data, you can only really guess. I don’t know if it’s good, if it’s bad or if there’s no effect. I still think there should be some caution involved or let’s just be conservative and say hey let’s not just blast everybody with X-rays because we don’t know what it’s doing, could be good, could be bad, it could have no effect, but there should be some clinical or critical thinking involved before you plan to take an X-ray.
Dr. Joshua Eldridge: I like that. That’s a good way to leave that one. I think that’s a good way to go. So just be smart. Once we’ve taken the X-ray, how do we make sure we’re not missing anything? So you got the X-ray, let’s just say a lumbar spine. We got a lumbar spine X-ray and it’s up here in front of us, either on our monitor or on the viewer, what process do we have to go through to make sure that as clinicians, we don’t miss anything?
Dr. Cliff Tao: Well, I think it’s a good idea to have a checklist. The longer the checklist, the more thorough you are. I think everybody learned what I learned in school and what I learned in residency too were the ABCS, and that goes for spine and most other bone or musculoskeletal types of X-rays. Everybody knows A is for alignment, B for bone, C is for cartilage or joint spaces, and S is for soft tissues. That’s a good place to start, but then we have to realize there’s a little more under each letter. We could go further into it.
Dr. Joshua Eldridge: Go for it. Tell us about alignment.
Dr. Cliff Tao: Alignment, that’s probably the easiest one. Just making sure the bones line up on each view and then that’s kind of the reason why we got to have the right views first of all, and everyone knows this again, you got to have an AP and a lateral. Earlier before we started, I was saying I had a pediatric ankle fracture. I’ve seen a few of these where the fracture only shows up on one view especially in the ankle. It must be that it’s just more common, but I think it showed up on the lateral view, not on the A to P and not on the oblique view even. We got to have at least two or maybe even three more views to have a more thorough assessment. Alignment is make sure all the bones line up. B of course for bone and naturally, we think of bone density to start with.
That in itself is as hard to evaluate because the X-ray is not really for looking at bone density, it’s more looking at the anatomy. We know we need at least 30% to 50% loss of bone density in order for us just to identify it on X-ray. It’s worse in the spine by the way, so that number 30% to 50% is average for all the bones in the body, but in the spine and in particular, the lumbar spine, I think that number’s 70% to 80%, so it’s actually pretty bad in the lumbar spine. We have to kind of keep that in the back of our mind. The other things that are under B are the shape of the bone, it’s the shape or the morphology of the bone, and does that look okay. Are there little osteophytes here and there, are there erosions, is there sclerosis for example when describing a fracture.
This is more important if you’re communicating with the orthopedist or someone who’s in between the fracturing or they want to know the prognosis of the fracture. How close are the ends? Are they opposed, is there displacement, angulation, rotation? Is there a fragmentation? All these things are covered under B and in this specific example under if there’s a fracture. C is for cartilage or soft joint spaces. So you just think of for example, in the spine, the disc, there’s cartilaginous end plate or the annular fibers and then there’s the nucleus pulposus. You gotta look at those things, although we can’t really see them, but there’s ossification or calcification with them, we can comment on it as indirect relation to what we know is there.
Of course, the disc spaces can be increased or decreased, of course, most commonly, they’re gonna be decreased much more commonly than increased. Then is there abnormal change in the joint space? So in the spine, is there a wedging one way or the other, laterally, medially, what-have-you. There’s other areas where there’s cartilage too. So the other joints, so like the hip joints and the lumbar spine, or the symphysis pubis, all those joints that have cartilage that really look like spaces, but they’re not. Then S, I feel like a lot of people just gloss over the S because we really don’t see soft tissues that well on an X-ray, but on a well exposed or X-ray that’s done with good technique, you can see quite a bit of soft tissues and you can get a lot of information from them.
But we do of course have to realize that there’s a lot of stuff we don’t see on X-ray and there’s other stuff that we can use to evaluate the soft tissues, like a CT scan, ultrasound or an MRI, but just don’t forget to look at the soft tissues. Note any for example, common ones, atherosclerosis which everyone has seen in the abdominal aorta, but you can get that in the carotid sinuses in the neck, you can get in the upper vertebral arteries, you can get it in the ankle and the wrist which could indicate diabetes. That’s common in the soft tissue realm. How’s that?
Dr. Joshua Eldridge: That’s good, and swelling too, maybe soft tissue? Did you hit that one?
Dr. Cliff Tao: No, I didn’t mention it, but yeah that’s a good one too. Hard to see that directly, but easy to miss if you don’t look for it, but yeah we see that not infrequently for example in the knee, suprapatellar swelling or in the anterior wrist. Lot of times it’s just there’s a fat pad that looks a little deviated, some type of an indirect assessment of that.
Dr. Joshua Eldridge: That’s really good, and I think that that’s a good review because people forget and they’re just out there looking at X-rays and they’re looking if they do Gonstead, they’re just drawn on it for their manipulations or whatever they’re doing, and then they forget about all the important stuff that might be in there as well. I like the checklist idea. That’s just like a pilot where people’s lives are a little bit more important, but making sure you go through that each time. Cliff, get into the how you write a report then. We’ve gone through the ABCS, and get into how you write a report on that? What’s the different components to report, what should be on there legally. From a legal standard, what do you need to have?
Dr. Cliff Tao: Well, I think everyone knows this, but you gotta have the patient information at the get-go. So, patient name, date of birth, their gender, the date of the X-ray and of course, a date that you’re doing your report. I like to have a little bit of clinical indication in there, why you took the X-ray or maybe there’s something on the X-ray that looks a little funky to you. Also, sometimes, I like to put where the X-ray was taken if I know it’s not taken at the doctor’s office. In med-legal cases, sometimes it matters I think where the X-ray was done. For example, if the X-ray study was not great quality, who do you blame? The chiropractor or do you blame the Imaging Center? I think that matters too. Then you get into the meat of the X-ray report. Basically, there’s two sections in the meat, so there’s the findings section and there’s the impression or conclusion.
In the findings section, generally speaking, this is just what we see. It’s kind of the nitty-gritty, do I see a white thing, do I see a dark thing, was it round, was it square? Is it pointy? That’s where you go to town on describing what you see. Actually even before we get there, or right before we get there, I like to look at X-rays twice. I think the first time you look at an X-ray should be without any biased information. You just kind of forget about what the patient is in for, whether they have pain or not, if you can forget about what they look like. All that stuff is all extra information to me. Just look at the image for what it is, just the image and that will force you to be a little more objective, I think, and it’ll force you to look at the whole image which you should be looking at anyway. Then, you got to kind of reinsert that information back in your brain, Oh, okay. They came in because they’ve had back pain for three years, and they fell 10 years ago or whatever.
That should kind of focus you into a particular area and maybe it’ll change your report, maybe it won’t. A lot of times, it does. It takes a little bit longer I think to read an X-ray that way, but I think it’s a little more thorough and a little more objective that way. I do that and then you write it down, the nitty-gritty, what you see in the findings section. Then in the impression or the conclusions, that’s what you think of the findings. It’s what you think of what you just saw. Are they all normal things that you just saw, or is it degenerative disease? Is it spondylosis? Is it a fracture? And then kind of a subset of the conclusion or impression section is at least for me, recommendations. Are there further things you can do to figure this out? Do you need to take another X-ray view? Do you need to take the other side, or you need to get a CT scan or something? That’s where all that information goes. Then, of course, you have to sign the report at the end and I think that’s it.
Dr. Joshua Eldridge: All right, nice. Then once you’re done with everything, how do you build it back into your clinical relevance with the patient? I know as a radiologist, you’re just kind of sending it back and you’re giving your two cents on it, but then what about if it’s your patient? How do you kind of build that all back into your treatment plan, and how do you present it to the patient?
Dr. Cliff Tao: Well, I think you can do it a few different ways. One way is just to kind of show your patient the report. I think it probably depends on what’s on the report and what or how you perceive your patient to be. Do you really need to have your patients know every little detail about their X-rays, and is it gonna make that much of a difference? Those are things I think can be determined on a case-by-case basis. This is not a familiar scenario to me, so I think if it was me, I would wanna know. It takes more time obviously for the doc to kind of go through all these findings and hopefully they can sort out what’s relevant and what’s not relevant, and hopefully, the patient will have a little more confidence in treatment plan that the doctor’s proposing. Generally speaking, I use it to either refute or confirm your suspicions before the X-ray and maybe it’ll help you support your proposed treatment plan or management plan for the patient.
Dr. Joshua Eldridge: I know that for me, whenever I have radiology on the patient, let’s say lumbar spine, or there’s some spondylosis on there, and I’m able to say that’ll change my diagnosis code from something like lower back pain to actual spondylosis. Now it also increases your medical decision making like we talked about in podcast 2 and 3 with Warren Jahn, but that’s part of your assessment too. It’s gonna increase your medical decision making that you’ve looked at this X-ray and now you’re giving them a diagnosis of spondylosis or spondylosis with radiculopathy. It changes that hierarchy of your diagnosis codes. That’s a big deal when you’re talking about reimbursement because you wanna make sure that you get paid for what you’re doing. If someone brings in their X-rays from a previous chiropractor and they were more let’s say, subluxation based and you took the time to read through the X-rays, and you see that there’s something abnormal that might be something as well to justify your treating the patient to a third party as well.
Dr. Cliff Tao: Right, of course.
Dr. Joshua Eldridge: Tell me about your services that you provide. How does that work? When I’m in my office and I take an X-ray, how does Dr. cliff get my information to read my X-rays?
Dr. Cliff Tao: Well, it’s not that complicated. In my typical chiro that I serve, they have an X-ray in their office, they’re digital X-rays. There are several ways of getting the digital X-rays to me, so we set that up. It could be as easy as, soon as the X-ray is done on their end, they’re done taking the X-rays, they might have to hit one or two buttons and the X-ray gets sent over to me. It shows up on my computer within about 5 to 10 minutes, and I see it immediately. I can do it right away. Typically it takes us, meaning I also have a few associates here, or not here, but out there. It takes us about 24 to 48 hours to generate a formal report and get it back to you.
Actually, some of my guys have it set up where they just want a more routine process. I think they have a higher volume maybe of X-rays so it’s worth it to them. They have it set up, so it actually doesn’t take them anytime to send me the X-ray. The computer knows as soon as the study is done, it gets automatically sent to me. That way, they don’t spend any time trying to figure out how to send the X-ray to me when to send it, which studies to send, it just gets done automatically. I have a few guys like that as well. Most of my guys are, they send on just a case by case basis. They see something weird, they’ll send it to me, or if it’s maybe a complex case, then they don’t get it. But it’s not that hard. Once you get it going, it’s an easy process to send the study over.
Dr. Joshua Eldridge: Why would me as a chiropractor serving my city or my tribe here, why would I wanna send you my X-rays? What is the benefit to having a specialist look at my X-rays?
Dr. Cliff Tao: Well, I mean you could look at it a few different ways. I think it’s better, you get a more accurate report off of the X-rays. I’m probably thinking more of an idealistic situation. If it was your eye and we went to just a medical doctor and they took X-rays in our office, when you want a specialist look at your X-rays rather than– We’re all trained to read X-rays, but I just happen to have a little more training and it’s what I do all day. I think it just gives a higher level of service and professionalism to your practice. It could help streamline things too. I think it’s hard when chiropractors in a busy practice, they’re taking X-rays and they’re reading them. You might read a lot of X-rays, but I’ll tell you, there’s a lot of different things that I see on X-rays and that I don’t see on X-rays that chiropractors don’t see, or do see and then I don’t see them.
There’s over calls, there’s under calls. I’m talking ideal practice here, but we would like to try to minimize false negatives and minimize false positives. Then there’s special cases like med-legal cases. I think it always helps to get another chiropractor or another healthcare practitioner on the case. It just helps kind of spread the liability. I hate to say it, but it does spread the liability a little bit, but it also shows that we know what our limits are. When it comes to complicated X-ray that you have someone to send it to and do a more thorough job looking at it.
Dr. Joshua Eldridge: Alright, that sounds good. I know you do a case online, you put a few up on Facebook every now and then and people should definitely check that out. What are the percentage in your experience that chiropractors that are doing their own X-rays are missing things? And use me for an example. I don’t mind. I got broad shoulders, so I can take it. But if I got 10 X-rays, how many of those am I missing something on?
Dr. Cliff Tao: Oh, you know it’s very variable. I hate to say this, but for you, you probably wouldn’t miss a whole lot. It’d be probably less than one. Actually, it’d be probably more than one, but of the things that you miss, then you gotta look at does it really make a difference? Okay, so you missed a little osteophyte at L-1. Is that gonna make a difference? Probably not in your practice, but it might make a difference in someone else’s practice, so it’s hard to say. I do have some chiros that I think seem to miss on every single X-ray. I’m not gonna give any names, but I we’re all over the map.
There’s some guys that do very well at reading X-rays, but they send me all their X-rays because they kind of know that there’s a lot of stuff that goes on that they don’t really see if they’re not trained or reading them on a regular basis. Then I have guys that send me stuff but almost on every image, I gotta make a special call to them or special email to them to make sure they saw something. Those happen frequently. I don’t really know exactly how it impacts the patient in the end, but I’d say at least maybe on average, maybe 20% would have a significant impact on how you’re gonna treat the patient.
Dr. Joshua Eldridge: To me, that’s a big deal. 20%’s a big deal when it comes to treating a patient. That’s a lot to miss. Of those 20%, some of that could be like we just talked about in osteoma in the skull.
Dr. Cliff Tao: Yeah.
Dr. Joshua Eldridge: If you missed something like that, that could be the patient’s life at some point.
Dr. Cliff Tao: Right, yeah. It’s not a best-case scenario that the chiropractor would be adequately trained to read all imaging, but it’s hard to be good in everything. There’s some guys out there that they’re really good with all that stuff, but I tell a lot of my chiros, hey, I don’t talk to your patients. You should be looking at the X-rays that you take, but maybe from a preliminary standpoint, and then you send it to me. You and I can talk about it but in the end, I should be doing that final analysis or final report on the X-rays. I hate to bring this into it, but from a med-legal standpoint, if you ever get subpoenaed for your records or whatever and you’re the last, why didn’t you just send this to a radiologist to read? There’s rarely a good answer for that, at least that I’ve seen. I think it’s good in the end. I know I’m kind of talking from an idealistic standpoint, but from a perfect scenario, we’d have a specialist doing everything, but we’re not in a perfect world.
Dr. Joshua Eldridge: Right, so if people wanna find out more about your services, where do they go to find out more about your services? How can they get ahold of you?
Dr. Cliff Tao: Oh, well they can go to my website. Should I give you the website?
Dr. Joshua Eldridge: Yeah, go for it.
Dr. Cliff Tao: Okay, it’s www.clifftaodcdacbr.com.
Dr. Joshua Eldridge: Tao is T-A-O. Just so people know that. C-L-I-F-F T-A-O.
Dr. Cliff Tao: Yes, same thing on Facebook. I’m pretty active on Facebook so you could search me with Cliff Tao, DC DACBR, and same thing on LinkedIn as well, or they can call me, 714-876-1126. I might not pick up the phone, but at least you can call me, and I’ll call you back eventually.
Dr. Joshua Eldridge: Now, the other cool thing that you do, you do a really cool event that just happened last weekend. It’s an amazing ski trip that you do up at Mammoth Mountain each year. Tell us a little bit about what you do and what kind of time it is for those chiros that come out there.
Dr. Cliff Tao: Alright, we’ve been doing it for about seven years now, just had it last weekend. It’s always at Mammoth Mountain. Obviously, Josh, I love to ski. That’s one of my passions, but so is chiropractic. They say you should work smarter, not harder so I’ve combined two of my passions for a two-in-one weekend where you can get continuing education and some great skiing in. What I do, I bring in a few speakers that I know, that do a good job. It’s kind of a mishmash all over the place. This past year, we had a great guy talking about documentation, another guy talking about personal injury, another guy talking about pediatric adjusting and a neurology guy, a neuro diplomate talking about his neuro exam and stuff like that. It’s kind of different guys and gals talking about their specialty within chiropractic. I try to keep it pretty formal on the CE, or not formal, but we’re dressed very informally because we’ve just gotten off the ski lifts or something, but we do have food there. It’s generally a pretty good time.
Dr. Joshua Eldridge: That’s pretty cool. They find more information about that at your website as well?
Dr. Cliff Tao: That’s on my website as well, yeah.
Dr. Joshua Eldridge: Perfect. That’s something that I am very much looking forward to. I really wanna come out this next year and come to your event and hang out. The last time me and you skied together was in Michigan when you broke your fibula.
Dr. Cliff Tao: Yes, boot top fracture.
Dr. Joshua Eldridge: Yeah, I remember that one.
Dr. Cliff Tao: I had no insurance by the way.
Dr. Joshua Eldridge: Back in the day, huh?
Dr. Cliff Tao: Yes, I have insurance now.
Dr. Joshua Eldridge: Just in case it happens. Are you still doing the crazy stuff down the slopestyle? Are you coming down and hit the tabletops and all that kind of stuff?
Dr. Cliff Tao: No, I don’t do those anymore, Josh. I’m a little too risky now, and I’m a little more fragile now. I stay off those things. I do get a little bit of air, but not much air these days. Yeah, I would love to have you come out and it’d be a great time. Yes, it’s fun times. A nice little venue and just a small group of guys. Usually, we have about 20 people, probably a little more next year maybe, but good skiing and you can learn a couple things, and hopefully get some CE in there too.
Dr. Joshua Eldridge: Nice, well, Cliff, thanks for joining us on the ChiroPractice Pro podcast. I really enjoyed having you, and thanks for taking the time and sharing your knowledge about radiology.
Dr. Cliff Tao: You’re very welcome, Josh. Thanks for having me.
Dr. Joshua Eldridge: All right, you bet. Thank You, Cliff, for joining us on the ChiroPractice Pro podcast. Don’t forget to download your free X-ray review checklist and see the example X-ray read at chiropracticepro.com/episode7. We enjoyed having you on today’s episode, and we hope that you found real value with the podcast. If the ChiroPractice Pro podcast has helped you in your practice, take a moment and leave a review on iTunes and then share with another chiropractor that you respect. From our team here at ChiroPractice Pro, we want to say thank you in advance for doing this. Don’t forget that to be successful in practice, it’s all about the little things. Keep doing the little things each day to see big results. We’ll see you next time right here at chiropracticepro.com.
11 episodes
All episodes
×Welcome to Player FM!
Player FM is scanning the web for high-quality podcasts for you to enjoy right now. It's the best podcast app and works on Android, iPhone, and the web. Signup to sync subscriptions across devices.