REBEL Core Cast 116.0 – Achilles Tendon Rupture
Manage episode 397396669 series 3435728

 Take Home Points
Take Home Points
- Achilles tendon rupture is a clinical diagnosis. The Thompson Test should be applied in all suspected cases.
- Remember to brace or splint a rupture, even if suspected, in the resting equinus position for optimal healing and prevention of further injury.
- Schedule follow up with orthopedics within 1 week for discussion of operative management vs early rehab protocols.
REBEL Core Cast 116.0 – Achilles Tendon Rupture
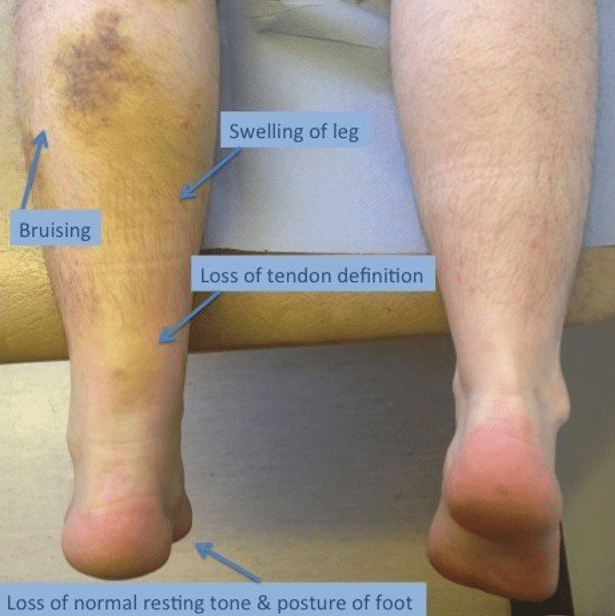
Physical Exam
- May have palpable gap or deformity in region of tendon.
- Weakness with plantar flexion.
- Increased resting ankle dorsiflexion on affected side in prone position with knees bent .
- Usually in absence of bony tenderness unless accompanied by other injury
- Thompson Test (video)
- Place the patient in the prone position, with feet hanging over the end of a stretcher or table. If patient is not able to lay down/there are no stretchers, the patient can kneel on a stool or chair
- Squeeze the calf of the normal limb. You will notice the squeeze will cause the ankle to plantarflex appropriately
- Squeeze the calf of the limb with the suspected Achilles tendon rupture. You will notice the squeeze will cause no motion if there is a full rupture/tear, and diminished motion if there is a partial tear
- Performance Characteristics (Garras 2012)
Sensitivity | Specificity | (+) LR | (-) LR |
96-100% | 93-100% | 13.7 | 0.04 |
Imaging
- X-Rays
- Used to rule out other or concurrent pathology
- May show soft tissue swelling and destruction of pre-Achilles fat pad (Kager’s Fat Pad)
- Findings are non-specific as tear of tendon unable to be visualized
- Ultrasound
- Ultrasound is helpful if obvious findings present and to distinguish between partial vs complete tears, however only around 50% sensitive for detecting only partial tears (Kayser 2005)
- MRI
- Gold-standard imaging modality
- Rarely, if ever, necessary in the ED
- Used for equivocal physical exam/alternate imaging findings or for assessing the severity of the tear for possible operative management
- Findings
- A full-thickness tear often shows a tendinous gap filled with edema or blood
- Complete rupture shows retraction of tendon ends
ED Management
-
- Provide analgesia
- Tendon stabilization in an optimal healing position
- Functional bracing/splinting in resting equinus/talipus equinus
- AO splint/brace in 20 degrees of plantar flexion for 4-6 weeks (may use tall CAM boot with 20 degrees wedge inserts)
- All patients should be non-weightbearing
- Any weight-bearing can convert a partial tear to a complete tear
- Maintain non-weightbearing status until see orthopedics (within 1 week)
- After evaluation by orthopedics, early weight-bearing and early ROM exercises yield better outcomes (can be as early as 2 weeks)
- Referral to rehab warranted to improve plantar flexion and decrease risk of re-rupture
- ED Ortho consultation: patients with open wounds in the area of trauma, or with concomitant fractures
- Operative Management is usually reserved for acute ruptures (approximately <6 weeks) of full thickness with large tendon gaps, failed conservative treatment of partial thickness tears, or high performance athletes
- These cases will be determined during follow up with orthopedics and may warrant outpatient MRI to assess severity of tear
Prognosis
-
- For conservative management, there is no significant difference in plantar flexion strength (Willits, 2010)
- Some increased risk of re-rupture compared to operative management, although review of evidence shows that this may not be significant if patients used structured, accelerated rehab protocol.
- Protocol includes initially non-weightbearing cast with the foot in equinus position as described above, then transitioned to a pneumatic walker with elevated heels (elevation gradually reduced biweekly), and physical therapy to improve gait, strength, and mobility. (Wallace 2011)
- If addressed early and appropriately, most patients have good self-reported long-term outcomes regardless of the treatment modality
Links
Orthobullets: Achilles Tendon Rupture
Resources:
- Sheth U et al. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: a population-based study of 27,607 patients. Bone Joint J. 2017; 99-B(1): 78-86. PMID: 28053261
- Chiodo CP, Wilson MG. Current Concepts Review: Acute Ruptures of the Achilles Tendon. Foot Ankle Int 2006; 27(4): 305-13. PMID: 16624224
- Leppilahti J, Orava S. Total Achilles tendon rupture. A review. Sports Med. 1998; 25(2): 79-100. PMID: 9519398
- Kayser R et al. Partial rupture of the proximal Achilles tendon: a differential diagnostic problem in ultrasound imaging. Br J Sports Med. 2005; 39(11): 838-42. PMID: 16244194
- Margetic P et al. Comparison of ultrasonographic and intraoperative findings in Achilles tendon rupture. Coll Antropol. 2007; 31:279-284. PMID: 17598414
- Garras DN et al. MRI is Unnecessary for Diagnosing Acute Achilles Tendon Ruptures: Clinical Diagnostic Criteria. Clin Orthop Relat Res 2012; 470(8): 2268-2273. PMID: 22538958
- Willits K et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation .J Bone Joint Surg Am. 2010; 92(17): 2767-75. PMID: 21037028
- Wallace RG et al. The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture. J Bone Joint Surg Br 2011; 93(10):1362-6. PMID: 21969435
- Erickson BJ. Is Operative Treatment of Achilles Tendon Ruptures Superior to Nonoperative Treatment? Orthop J Sports Med. 2015; 3(4): PMID: 26665055
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter/X: @srrezaie)
The post REBEL Core Cast 116.0 – Achilles Tendon Rupture appeared first on REBEL EM - Emergency Medicine Blog.
15 episodes




